Where are they now? Two women associated with the early days of the pandemic look back a year later
March 12, 2021
‘We pulled together’
Kimberly Blanton was on her way home when she got the call that made the pandemic real.
“I knew the minute I got the call from the governor’s office that that first patient was positive here,” Blanton said. She turned her car around and went back to work.
Blanton, MSN, RN, MHA, is director of Infection Prevention and Control for UK HealthCare. In the early days of the pandemic, she was one of the people responsible for the behind UKHC’s COVID-19 response – checking PPE supply levels, coordinating cross-office initiatives and sometimes speaking at press conferences to inform the public about this new disease and its ramifications.
“I’d get off from doing the interview and then two hours later, something would change in the guidance,” Blanton said. “And so I know I remember calling people routinely, I kind of felt schizophrenic at a time because it was changing so quickly, because we were learning as we were going.”
Prior to Kentucky’s first case of COVID-19, Blanton worked with the campus team extricate students who were studying abroad. That was where she first ran into an issue that became a hallmark of the early pandemic period – medical supply shortages.
“We couldn’t get a thermometer for students. There were no thermometers in town,”
Blanton said. “I thought ‘well, I have never.’” She recommended UK’s Emergency Operations Center begin stockpiling thermometers for students.
At the hospital, Blanton was strictly managing protective equipment through a centralized station that she kept in place until July.
“It was more or less, real stressful, because you were trying to make sure you had what, what you needed and that we were moving quick enough to get the supplies in and find other supplies that we could substitute because they were backordered,” Blanton described. Part of this shortage came from limited manufacturing, but also competition from other states that Blanton said led to an ‘unheard of’ shortage.
She would quickly take on another crucial role – being the voice UKHC’s COVID-19 approach by personally calling individuals who tested positive.
For the first several months, I called every positive patient back myself, worked through the list myself, while the other members of my team, were just building calls and dealing with supply issues,” Blanton said, which could be hours of work.
“They’re scared,” Blanton said. “You have to talk with them and help them and give them direction.”
Fortunately, the infectious disease team had just undergone refresher courses for viral diseases in November with a crop of Ebola experts.
“That was beyond valuable,” Blanton said. “It was a totally different virus and how we handled it, because this was so completely respiratory driven, but it was so handy to have had that experiences and run those demos.”
Good partnerships, not just with state offices, but with the clinic side of UK healthcare, helped manage the transition to full-blown pandemic.
“We were able to send people when they, you know, if you didn’t need to be in the hospital, but you still needed to be seen via telehealth, or we needed to get to COVID swabbed or get your medicines, whatever, we were able to really have a great partnership,” Blanton said.
Though prepared for an influx of patients, Blanton said she did ‘not at all’ expect the scale and extent of COVID-19 in the U.S.
“I never dreamed, ever, that we would be sitting here today talking about a year of a pandemic like we’ve been through. I suspected we would have a few cases,” Blanton said. “I never dreamed it would be this way.”
The scale of sickness has taken a toll on healthcare workers, which Blanton has witnessed firsthand.
“Your job is to help those who are in need. And we do it, and we do, you know, we’re a trauma
“For the first several months, I called every positive patient back myself, worked through the list myself, while the other members of my team, were just building calls and dealing with supply issues,” Blanton said, which could be hours of work.
“They’re scared,” Blanton said. “You have to talk with them and help them and give them direction.”
Fortunately, the infectious disease team had just undergone refresher courses for viral diseases in November with a crop of Ebola experts.
“That was beyond valuable,” Blanton said. “It was a totally different virus and how we handled it, because this was so completely respiratory driven, but it was so handy to have had that experiences and run those demos.”
Good partnerships, not just with state offices, but with the clinic side of UK healthcare, helped manage the transition to full-blown pandemic.
“We were able to send people when they, you know, if you didn’t need to be in the hospital, but you still needed to be seen via telehealth, or we needed to get to COVID swabbed or get your medicines, whatever, we were able to really have a great partnership,” Blanton said.
Though prepared for an influx of patients, Blanton said she did ‘not at all’ expect the scale and extent of COVID-19 in the U.S.
“I never dreamed, ever, that we would be sitting here today talking about a year of a pandemic like we’ve been through. I suspected we would have a few cases,” Blanton said. “I never dreamed it would be this way.”
The scale of sickness has taken a toll on healthcare workers, which Blanton has witnessed firsthand.
“Your job is to help those who are in need. And we do it, and we do, you know, we’re a trauma center, and we take care of some traumatic things,” Blanton said. “And it’s always placed on you. I mean, it just lays heavy on your heart.
Though there were hopeful times, like the release of the COVID patient and her husband, healthcare workers were under constant stress, including witnessing the pain of separated families.
“That was so heartbreaking. It’s hard to not be able to have families, and sometimes we had husbands and wives that were sick and they were two doors apart,” Blanton said. UK was able to use their E-ICU units to connect patients with families virtually. Blanton thinks telehealth and infection control practices are here to stay.
“One would have thought that would have been how we would always be thinking, but people now know hand hygiene, mass, social distancing, they work,” Blanton said.
Those practices have worked to mitigate cases, Blanton said, but real hope arrives in the form of vaccines.
“For us in infection control, we have absolutely seen a decrease in the numbers since we rolled out the vaccine,” Blanton said. That effect will hopefully bring the pandemic under control by the end of the year.
In the meantime, Blanton is encouraged by people stepping up to help others. She is especially thankful for community members who donated supplies to the hospital.
“When I think back on this year, if I’m ever blessed have grandchildren, I’ll be able to say ‘boy, I lived through this.’ And it was hard times. But the thing I saw was that we, we pulled together.”
‘Definitely a roller coaster’
The pandemic began sooner for Kaitlyn White than it did for many other Americans.
White, 23, was the first UK student publicly revealed to have COVID-19, testing positive on March 25, 2020. She’s since had COVID-19 a second time, but didn’t get as sick, and is now vaccinated.
“When I found out I had it a second time I was like, ‘Oh no, here we go again,’” White said.
Looking at the millions of Americans who have contracted the virus since then, White said being one of those early cases is “unreal.”
“The first time, it was a big deal. It was like, ‘Oh god.’ But now, almost every time I log into social media I see a new person say, ‘Oh yeah, positive now I have to quarantine.’ And it’s almost like this, like for them it’s just a nuisance, it’s not, it’s not a big deal.”
Knowing that White had COVID-19 early on, friends have reached out for suggestions when they contracted the virus. White finds it strange how many people act casually about the virus.
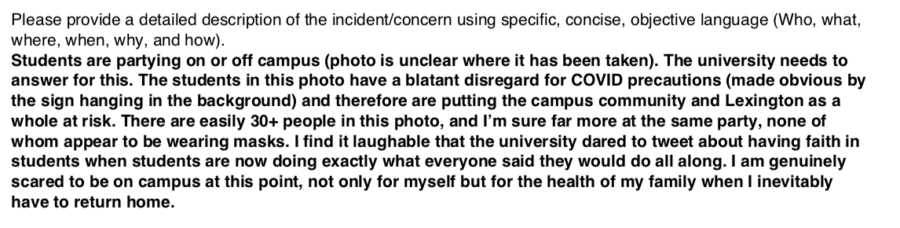
“There are so many people who are insisting on partying insisting on going out to bars, insisting on living like we’re not in the middle of a pandemic, and I can’t,” White said. In her original interview with the Kernel, White said she was vocal about her positive result in order to raise awareness of the still-underestimated disease.
“The craziest part about it is, we would be done with this already. Like, we wouldn’t even be having this conversation if in March and April of 2020 we took the time to lock down and isolate the way we needed to,” White said.
White was one of the first 1,000 cases in Kentucky and likely one of the first 100 in Lexington.
“You still don’t see me out at bars. You still don’t see me out partying. I’m still wearing a mask, every time I’m in public. It’s just crazy how many people refuse to do anything to help,” White said.
White’s first bout with COVID-19 last March shaped her life in one significant way – she returned to UK for grad school after spending half of her final semester online and after graduating in 2020.
“I originally was not going to stay here, but I ended up feeling so connected to the UK community as a result of the professors and staff who reached out to me and made such an active effort to be in my corner and show me how much they cared when I was going through that.”
White is now earning a Master’s through the College of Education and has high hopes of walking at an in-person ceremony when she graduates with that degree. Her undergraduate degree earned in 2020 ‘doesn’t feel real’ because the ceremony was canceled.
White thinks that most of the COVID-19 cases among UK students were avoidable and happened because students intentionally ignore safety protocols.
“I think the university itself is in kind of a tricky situation, because they are obligated to provide us the best education that they can and for a lot of majors a lot of courses, programs, etc. Their material isn’t accessible virtually,” White said.
When students contract COVID-19 this year, they are reported to UK’s Health Corps. But when White got sick, that center did not exist yet. Help instead came from individual professors, checking in on her and her health.
“I was actually able to finish spring semester with a 4.0, even having COVID in the middle of the semester,” White said. “And the big reason I was able to do that is because my professors were so accommodating. So I’m eternally grateful for them, for helping me stay on track.”
White wishes UK would do more for students’ basic needs and is appreciative of the vaccine rollout. Her main reason for getting the vaccine was to protect others, since she has already had COVID-19 twice.
“I kind of had the same feeling as voting,” White said. “Like it to me It felt kind of like a civic duty.”
White said the one-year anniversary of COVID-19 in Kentucky feels like the end of a long roller coaster ride.
“One year ago, I had a completely different vision of what I would be doing with my life right now,” White said. The pandemic forced her to slow down, rethink her priorities and check in on her mental health.
“Before it’s like I was on a dead sprint. And I was so focused on that finish line that I wasn’t paying attention to the things I was passing,” White said. Now, she goes to therapy regularly and has taken stock of her physical well-being. And, White was able to accomplish the only goal on her mind during her first bout with COVID-19 – taking her dog and quarantine companion, Eli, to the dog park.
“I have had to look very very hard for a silver lining in all of this, and that is what I have found – is that this has given me the opportunity to slow down to focus on myself and to come out of this, one year later, stronger than I was.”