FDA uses UK researcher’s findings
February 5, 2013
By Melody Bailiff
A UK researcher’s findings on the drug hydrocodone were used by the FDA as testimony in the reclassifying of the drug that had 219 million doses dispensed in Kentucky during 2011.
The Risk Management Advisory Committee of the FDA voted Jan. 25 in favor of reclassifying hydrocodone from a Schedule III to a Schedule II drug under the federal Controlled Substance Act.
This reclassification would mean tougher restrictions on the prescribing and purchasing of the drug.
Dr. Sharon Walsh, director of the Center on Drug and Alcohol Research at the UK College Medicine, gave expert testimony at the January FDA hearings.
It has long been debated by the DEA whether or not this reclassification would help reduce misuse and trafficking of one of the most abused drugs in the nation.
Namely, this is one of the most abused drugs in Central and Eastern Kentucky with enough of the drug dispensed for each person in the state to have 51 doses.
Walsh, along with a team of researchers, conducted research on opiate users that came to UK hospital to study the comparative pharmacology of hydrocodone in comparison to drugs like Oxycontin and morphine.
The study looked at hydrocodone given intravenously compared to Oxycontin and morphine.
It was found that although hydrocodone was a Schedule III drug, it could not be distinguished from agents in Schedule II drugs. It was virtually identical in its pharmacological profile.
“It is interesting that the FDA asked me to come because the studies we conducted at UK are some of the first on hydrocodone over a course of many years,” Walsh said. “Those studies were a significant part of consideration of the committee and it shows the research has gone on to contribute to national decision-making process.”
Walsh said that data shows people who abuse prescriptions are getting opiates from friends or family members with prescriptions.
Data shows a smaller percent are using dealers, and the drug’s street-value has given an avenue for dealers to supplement their income as part of their prescriptions.
Some question if it is the patients who are the source of the trafficking, or if it is the doctors who prescribe the drug.
The Courier-Journal reported in 2011 that “pill mills” were the source problem in Central and Eastern Kentucky.
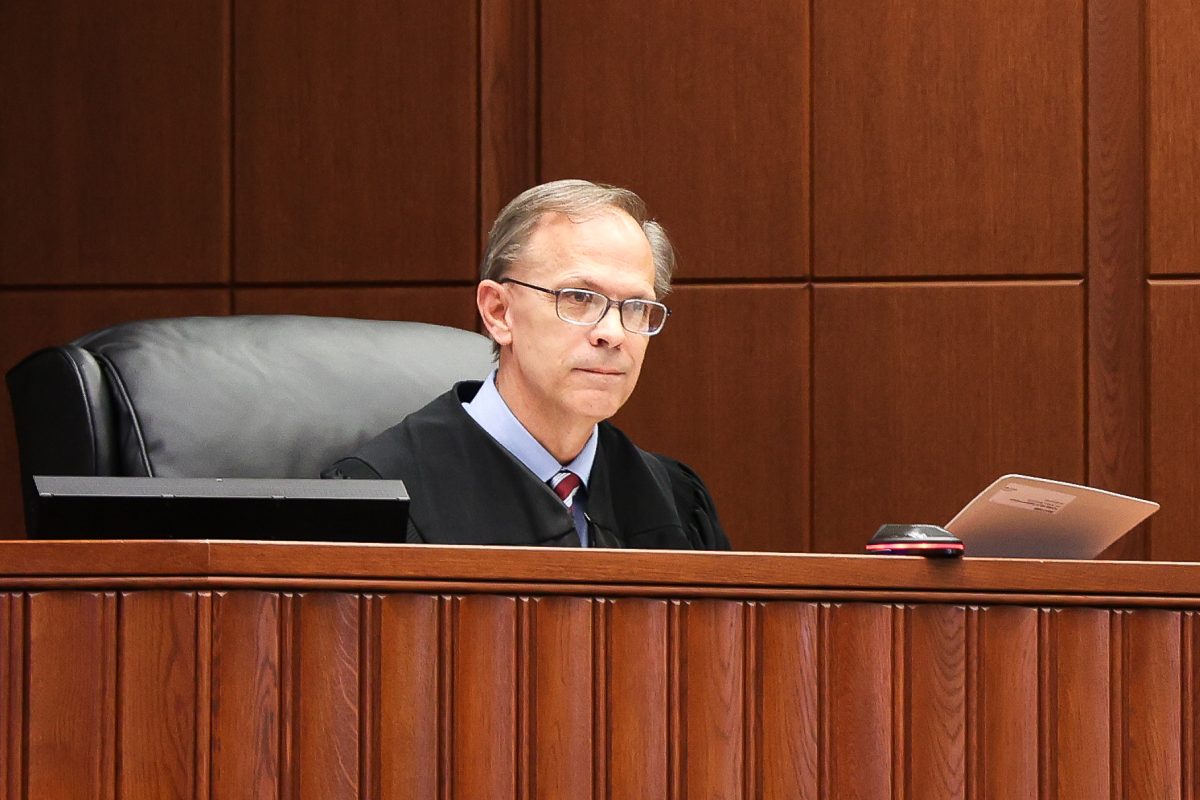
It was reported that Dr. Frederick Cohn of Greenup and Johnson counties in Eastern Kentucky dispensed more than 2.5 million tablets with a of controlled substances with a colleague, sometimes seeing 120 or more patients in a four-hour period, according to court records.
Dr. Cohn is one of many doctors in Eastern Kentucky that has been convicted for the practice of “pill mills” in the last ten years.
Paintsville Mayor Bob Porter stated in 2011 that pill mills are an epidemic that is killing the community.
“What we end up doing is arresting all these ‘victims’… and the doctors who create the problem continue to practice,” Porter stated in an interview with the Courier-Journal.
“In some places this will hurt people that need it. Laws vary by state and in most the requirements for Schedule II drugs are strict, you must have a paper prescription so you have to have a means to get to the doctor,” Walsh said. “Also the prescription for Schedule II are 30 days with no refills, opposed to a six-month supply a patient may obtain with a Schedule III prescription.”
Also to help regulate those who “doctor shop” to obtain prescriptions some states have instituted prescription monitoring programs.
These may reduce the amount of people who are not legitimate patients by alerting doctors if the patient has more than one doctor for prescriptions.
The procedures following the Jan. 25 vote will require the FDA to consider the recommendation of the committee and then propose its final recommendation to the DEA.
Walsh said it is impossible to predict the outcome of the DEA’s decision but something should be known in a few months.