Treatment Hope for People with Bipolar I Disorder Symptoms
April 6, 2022
(BPT) – Paid for by AbbVie
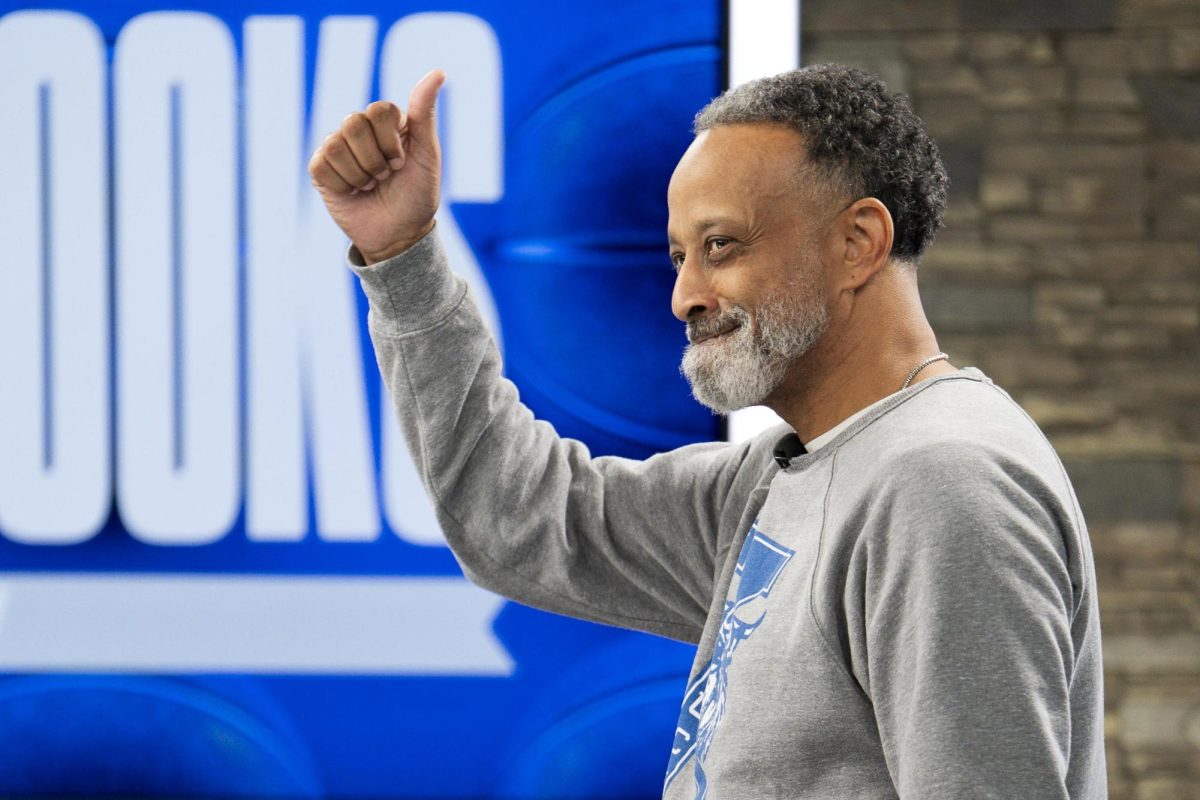
Matt Poldrugach, 44, is the owner of a Texas-based electric company and has been living with his bipolar I disorder diagnosis for several years. Matt believes it is more important than ever to have an open dialogue with your healthcare providers and loved ones to help reduce the stigma of living with bipolar I disorder and ensure people in similar situations have access to the resources, treatment and support they need.
Bipolar I depression symptoms can appear similar to the symptoms of major depressive disorder, including hopelessness, fatigue, extreme sadness and changes in appetite or weight. Manic symptoms, however, are specific to bipolar I disorder and can leave someone wired with racing thoughts and higher than usual energy levels. If you, like Matt, are diagnosed with bipolar I disorder, you’re familiar with unpredictable high and low mood swings that you experience during manic and depressive episodes.
It’s impossible to predict how long these mood episodes may last. You might be severely depressed for a brief or extended period of time before entering into a manic episode. You may even experience manic and depressive symptoms at the same time, which is known as a mixed episode.
As Matt knows, it can feel isolating to have bipolar I disorder, but it’s important to know you are not alone and there are treatment options available. Studies suggest that bipolar I disorder could affect around 3 million Americans at some point in their lives. Experts agree that effective treatment plans for people living with bipolar I often include a combination of medication, talk therapy, support groups, and improving overall health and wellness.
“I think there’s still quite a bit of a stigma, especially with bipolar,” Matt says. “I think some people might have perceptions that all patients with bipolar I disorder are violent and have uncontrollable actions, and that’s unfair.”
Exploring treatment options
Matt worked closely with his healthcare team to develop a treatment plan to help control his bipolar I symptoms. Like many people with bipolar I, it took Matt some time to find the right treatment for him.
“Finding the right treatment plan for you on your bipolar I journey is not easy – it’s difficult,” said Matt. “Don’t give up on yourself, work with your doctor, and listen to the advice of your healthcare providers to find a treatment that works for you.”
Many people with bipolar I disorder require medication as part of their treatment plan along with therapy and support groups. If you need help controlling your bipolar I symptoms, it’s important to ask your doctor about available treatment options.
Matt is greater than his bipolar I and so are you.
Through his journey to find an effective treatment to help manage the extreme highs and lows of his bipolar I, Matt started a medication called VRAYLAR® (cariprazine). VRAYLAR is a prescription medication approved to treat depressive episodes that happen with bipolar I disorder (bipolar depression) in adults and for the short-term (acute) treatment of manic or mixed episodes that happen with bipolar I disorder in adults. After his psychiatrist decided to prescribe him VRAYLAR, Matt notes that it helps him manage his bipolar I disorder symptoms, “Finding VRAYLAR has been a relief. It has helped smooth my ups and downs of bipolar I,” he says.
For more information about a treatment option, visit VRAYLAR.com. VRAYLAR is not right for everyone. Only your doctor can decide if VRAYLAR is right for you. Individual results may vary. To hear more from Matt and other real people’s stories with bipolar I, please visit https://www.vraylar.com/my-mood-matters/real-stories.
Please see the full Prescribing Information, including Boxed Warnings, and Medication Guide.
IMPORTANT RISK INFORMATION
What is the most important information I should know about VRAYLAR?
Elderly people with dementia-related psychosis (having lost touch with reality due to confusion and memory loss) taking medicines like VRAYLAR are at an increased risk of death. VRAYLAR is not approved for treating patients with dementia-related psychosis.
Antidepressants may increase suicidal thoughts or actions in some children and young adults within the first few months of treatment and when the dose is changed. Depression and other serious mental illnesses are the most important causes of suicidal thoughts and actions. Patients on antidepressants and their families or caregivers should watch for new or worsening depression symptoms, especially sudden changes in mood, behaviors, thoughts, or feelings. This is very important when an antidepressant is started or when the dose is changed. Report any change in these symptoms immediately to the doctor.
VRAYLAR may cause serious side effects, including:
- Stroke (cerebrovascular problems) in elderly people with dementia-related psychosis that can lead to death
- Neuroleptic malignant syndrome (NMS): Call your healthcare provider or go to the nearest hospital emergency room right away if you have high fever, stiff muscles, confusion, increased sweating, or changes in breathing, heart rate, and blood pressure. These can be symptoms of a rare but potentially fatal side effect called NMS. VRAYLAR should be stopped if you have NMS
- Uncontrolled body movements (tardive dyskinesia or TD): VRAYLAR may cause movements that you cannot control in your face, tongue, or other body parts. Tardive dyskinesia may not go away, even if you stop taking VRAYLAR. Tardive dyskinesia may also start after you stop taking VRAYLAR
- Late-occurring side effects: VRAYLAR stays in your body for a long time. Some side effects may not happen right away and can start a few weeks after starting VRAYLAR, or if your dose increases. Your healthcare provider should monitor you for side effects for several weeks after starting or increasing dose of VRAYLAR
- Problems with your metabolism, such as:
- High blood sugar and diabetes: Increases in blood sugar can happen in some people who take VRAYLAR. Extremely high blood sugar can lead to coma or death. Your healthcare provider should check your blood sugar before or soon after starting VRAYLAR and regularly during treatment. Tell your healthcare provider if you have symptoms such as feeling very thirsty, very hungry, or sick to your stomach, urinating more than usual, feeling weak, tired, confused, or your breath smells fruity
- Increased fat levels (cholesterol and triglycerides) in your blood: Your healthcare provider should check fat levels in your blood before or soon after starting VRAYLAR and during treatment
- Weight gain: Weight gain has been reported with VRAYLAR. You and your healthcare provider should check your weight before and regularly during treatment
- Low white blood cell count: Low white blood cell counts have been reported with antipsychotic drugs, including VRAYLAR. This may increase your risk of infection. Very low white blood cell counts, which can be fatal, have been reported with other antipsychotics. Your healthcare provider may do blood tests during the first few months of treatment with VRAYLAR
- Decreased blood pressure (orthostatic hypotension): You may feel lightheaded or faint when you rise too quickly from a sitting or lying position
- Falls: VRAYLAR may make you sleepy or dizzy, may cause a decrease in blood pressure when changing position (orthostatic hypotension), and can slow thinking and motor skills, which may lead to falls that can cause fractures or other injuries
- Seizures (convulsions)
- Impaired judgment, thinking, and motor skills: Do NOT drive, operate machinery, or do other dangerous activities until you know how VRAYLAR affects you. VRAYLAR may make you drowsy
- Increased body temperature: Do not become too hot or dehydrated during VRAYLAR treatment. Do not exercise too much. In hot weather, stay inside in a cool place if possible. Stay out of the sun. Do not wear too much clothing or heavy clothing. Drink plenty of water
- Difficulty swallowing that can cause food or liquid to get into your lungs
Who should not take VRAYLAR?
Do not take VRAYLAR if you are allergic to any of its ingredients. Get emergency medical help if you are having an allergic reaction (eg, rash, itching, hives, swelling of the tongue, lip, face or throat).
What should I tell my healthcare provider before taking VRAYLAR?
Tell your healthcare provider about any medical conditions and if you:
- have or have had heart problems or a stroke
- have or have had low or high blood pressure
- have or have had diabetes or high blood sugar in you or your family
- have or have had high levels of total cholesterol, LDL-cholesterol, or triglycerides; or low levels of HDL-cholesterol
- have or have had seizures (convulsions)
- have or have had kidney or liver problems
- have or have had low white blood cell count
- are pregnant or plan to become pregnant. VRAYLAR may harm your unborn baby. Talk to your healthcare provider about the risk to your unborn baby if you take VRAYLAR during pregnancy. If you become pregnant or think you are pregnant during treatment, talk to your healthcare provider about registering with the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or
http://www.womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/ - are breastfeeding or plan to breastfeed. It is not known if VRAYLAR passes into breast milk. Talk to your healthcare provider about the best way to feed your baby during treatment with VRAYLAR
Tell your healthcare provider about all medicines that you take, including prescriptions, over-the-counter medicines, vitamins, and supplements. VRAYLAR may affect the way other medicines work, and other medicines may affect how VRAYLAR works. Do not start or stop any medicines while taking VRAYLAR without talking to your healthcare provider.
What are the most common side effects of VRAYLAR?
- The most common side effects were difficulty moving or slow movements, tremors, uncontrolled body movements, restlessness and feeling like you need to move around, sleepiness, nausea, vomiting, and indigestion.
These are not all possible side effects of VRAYLAR.
Please see the full Prescribing Information, including Boxed Warnings, and Medication Guide.
US-VRA-210523 02/22