State attempts to curb prescription drug abuse
October 21, 2012
By Jessica Stokes
Prescription drug abuse and related topics have received much media attention lately. Unfortunately, a lot of that attention has spotlighted Kentucky.
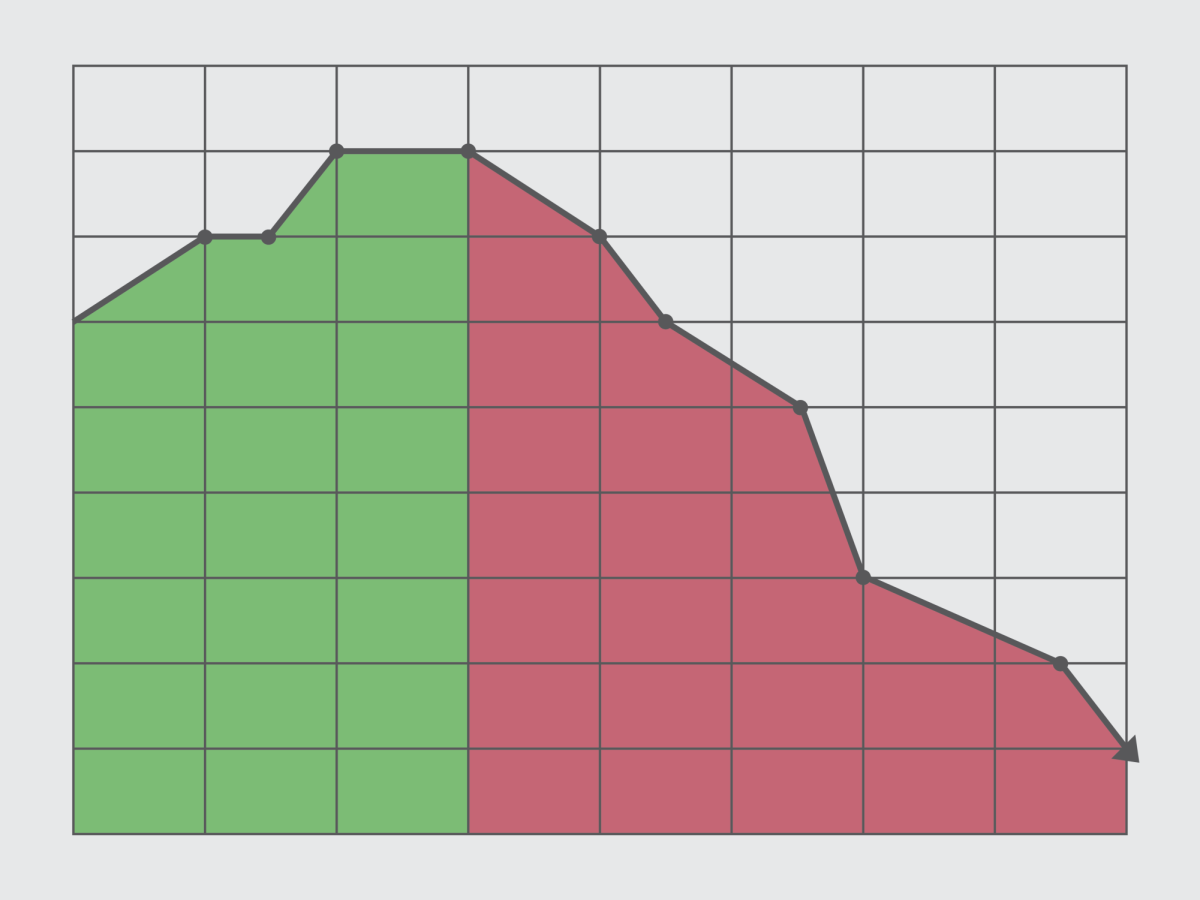
Several newspaper articles around the country have mentioned the fact that more Kentuckians died last year from prescription drug overdose than did in car accidents. While shocking at first, this fact doesn’t seem as surprising when considering that Kentucky’s opioid abuse rate is among the highest in the country.
Additionally, the highly publicized Florida pain clinics that were recently shut down due to unethical prescribing have contributed largely to the problem of prescription drug abuse in Kentucky, particularly in the eastern parts of the state.
With these sad truths creating a negative reputation for our state — and more importantly — ruining the lives of thousands of Kentucky families, something had to be done to combat the tragedy of prescription drug abuse.
House Bill 1, which went into effect July 20, was designed to address several of the underlying issues that are contributing to this devastating problem.
However, it is also important to note that this bill was not written with the intent to limit medication access for patients who have legitimate medical needs.
Kentucky All Schedule Prescription Electronic Reporting, keeps track of both prescribing and dispensing of scheduled medications for individual patients. KASPER, the statewide database specific to Kentucky, is similar to reporting systems that are being used in several other states. Although KASPER has been around for several years, HB-1 expanded its use by requiring all practitioners with valid DEA licenses, regardless of whether or not they prescribe controlled substances, be registered with KASPER in order to maintain medical licensure. HB-1 also ensures that the KASPER system will be used more than in the past.
Although many practitioners previously had access to KASPER reports, HB-1 ensures that the system is used by requiring that a KASPER report be run on initial prescribing of Schedule II or Schedule III products containing hydrocodone.
Furthermore, another report must be obtained every three months if treatment with these medications is to be continued. Keep in mind, however, that this does not mean that patients who have been treated by the same doctor for extensive periods of time will have gaps in care. Instead prescribers would judge these situations on a case-by-case basis and use appropriate treatment standards for these patients.
Several of the most extensive changes due to HB-1 relate to pain management clinics. Prior to HB-1, pain management clinics were allowed to be owned by anyone who wanted to open a business. Consequently, many of these pain management clinics were owned by people without medical backgrounds. Several pain clinics, with owners of both medical and non-medical backgrounds, began prescribing controlled substances unlawfully.
Acceptance of flat consultation fees in exchange for a standard cocktail of controlled substances allowed avoidance of insurance companies, large profits for owners and physicians, and the ability to easily run a business and see hundreds of patients per day.
Often, little consultation was actually provided and professional judgment was ignored when prescribing. Also, many pain clinics obtained their supply from smaller wholesalers that had more lenient rules about what they would sell when compared to the larger wholesalers such as McKesson or Amerisource Bergen. These suppliers would often allow orders to solely consist of controlled substances, obviously making their operations run more smoothly.
Now, under HB-1, only physicians can own pain management clinics. If unlawful prescribing is detected, physicians would not only be at risk of losing their businesses, but also their medical licenses. HB-1 also requires that pain clinics accept insurance as opposed to operating as cash-only businesses. As seen in the media with Florida pain clinics, many pain clinics stayed “under the radar” because regular insurance claims could not be filed. HB-1 will help to avoid this problem in Kentucky.
Lastly, and in addition to the increased monitoring and changes seen with pain clinics, HB-1 allows health-care professionals to incorporate KASPER reports into patient medical records. The information can also be shared with other health-care professionals involved in the patient’s care, as well as the patient themselves. Previously practitioners were not allowed to share this information. This often led to gaps in treatment and may also have contributed to increased abuse and diversion since all healthcare professionals involved with the patient were not aware.
Although the implicated changes seem strong enough to curb abuse and diversion, HB-1 has only been in place for a little over two months. At this point the impact of this legislation cannot be measured. Hopefully the implemented changes will make a difference in the lives of Kentuckians and slow the problem that has so dramatically affected our state’s families.